Antigen
Subunit vaccine proteins based on the S1 and RBD regions of SARS-CoV-2 were produced separately. Codon-optimized complementary DNAs encoding the S1 and RBD genes of the Wuhan-Hu-1 strain (GenBank: NC045512) were synthesized and cloned into the pcDNA™3.3-TOPO® vector (ThermoFisher, Waltham, MA. USA). Chinese hamster ovary (CHO) cells were transfected with each recombinant vector, and culture supernatants containing the expressed S1 or RBD proteins were harvested and purified for vaccine production. The vaccine formulation, manufactured by CTCVAC Co., Ltd, (Hongcheon, South Korea) contained 60 µg of S1 protein, 60 µg of RBD protein, and 10% Montanide gel PR02 (Seppic, Paris, France) as an adjuvant per dose.
Experimental design in laboratory animals
All animal experiments were conducted in accordance with the care and use of laboratory animal guidelines of Jeonbuk National University and were approved by the Institutional Animal Care and Use Committee (approval number: NON2022-05). Seven specific-pathogen-free (SPF) female beagle dogs (9 months old) were purchased from Orient Bio Inc. (Seongnam, Gyeonggi-do, South Korea) and housed individually in large-animal cages within a biosafety level 2 (BSL-2) facility at the Korea Zoonosis Research Institute. After a 2-week acclimation period, three dogs designated for vaccinated group were intramuscularly immunized with the SARS-CoV-2 subunit vaccine candidate on days 0 (first dose), 21 (second dose), and 49 (booster dose). The booster dose was administered following the same procedure as the initial two vaccinations. It was performed to ensure robust antibody response and to establish cross-protective immunity through the inactivated vaccine format26. In addition, based on our preliminary study (Additional file 5), two doses of the vaccine were insufficient to elicit adequate neutralizing antibody response, whereas a marked increase was observed only after administration of the booster vaccination. These findings supported the inclusion of a three-dose (first, second and booster dose) regimen in the present experimental design. Another three dogs designated for non-vaccinated group were injected intramuscularly with adjuvant alone, and one dog served as an uninfected negative control.
For the challenge study, all dogs were transferred to a BSL-3 facility certified by the Korea Disease Control and Prevention Agency (certification number: KCDC-15-3-02). Biosafety-related procedures were approved by the Institutional Biosafety Committee of Jeonbuk National University (approval number: JBNU 2022–11 − 001). The dogs were anesthetized with Zoletil50 and inoculated intranasally with 1mL of the SARS-CoV-2 Delta variant (NCCP 43390, B.1.617.2 lineage, 106.0TCID50/ml). The negative control dog received 1mL of DMEM intranasally. Each group was housed separately.
Clinical signs, body temperatures, and body weight were monitored daily for DPI7. Nasal and rectal swabs were collected daily for viral RNA detection, and blood samples were obtained on weeks 0, 3, 6, and on DPI0, 2, 4, and 7 for SN test and blood chemistry analysis (Fig. 5). Neutralizing antibody responses against the Wuhan strain were assessed by ELISA and SN tests without viral challenge, while challenge experiments focused on the Delta variant to evaluate cross-protection efficacy and adhere to the 3Rs principle.
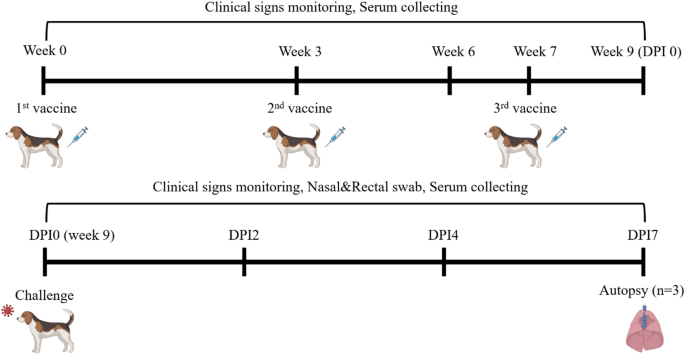
Schematic diagram of the SARS-CoV-2 infection experiment in laboratory animals.
After a 2-week acclimation period, three dogs were randomly selected and vaccinated intramuscularly on days 0 (first dose), 21 (second dose), and 49 (booster dose). Another three dogs, designated as the non-vaccinated group, received intramuscularly injections of adjuvant alone, and one dog served as a negative control. For the challenge study, dogs were anesthetized with Zoletil50 and inoculated intranasally with 1mL of the SARS-CoV-2 Delta variant (NCCP 43390, B.1.617.2 lineage, 106.0TCID50/ml). The negative-control dog received 1mL of DMEM intranasally. All dogs were monitored daily for clinical signs, body temperature, and body weight up to DPI7. Nasal and rectal swabs were collected daily to quantify viral shedding, and blood samples were obtained on weeks 0, 3, 6, and on DPI0, 2, 4, and 7 for SN test and blood chemistry analysis. The figure was created with BioRender.com, accessed on 2 February 2025.
Clinical trial in companion animals
The clinical trial involved companion dogs and cats divided into four groups: vaccinated dogs (n = 30), non-vaccinated dogs (n = 15), vaccinated cats (n = 30), and non-vaccinated cats (n = 15). All animals tested negative for coronavirus antigen by RT-qPCR prior to the start of the study (Additional file 6). The vaccination schedule was identical to that used in the infection experiment (Fig. 6).
CBC, blood chemistry, and SARS-CoV-2 antibody ELISA tests were performed seven days before the first vaccination and 14 days after the final vaccination to evaluate potential adverse effects and immunogenicity. To assess antibody persistence, ELISA were conducted at 4, 8, and 12 weeks post-final vaccination in 20 randomly selected vaccinated animals. Based on preliminary data indicating a decline in neutralizing antibody titers after 12 weeks and nearly being undetectable by week 16, the study monitored antibody responses up to 12 weeks post-final vaccination (Additional file 5). Additionally, 15 dogs and 15 cats (10 vaccinated and 5 unvaccinated) were randomly selected for SN test to confirm neutralizing antibody production.
All animal experiments complied with the current laws of the Republic of Korea. Animal care and treatment were performed in accordance with the guidelines established by the Institutional Animal Care and Use Committee (approval number: P22-001).
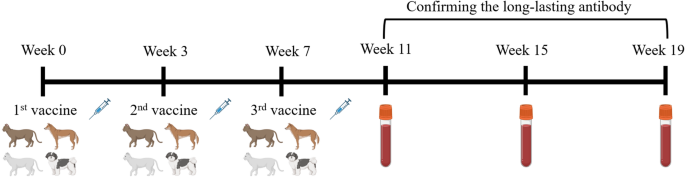
Schematic diagram of the clinical trial in companion animals.
The clinical trial included companion dogs and cats divided into four groups: vaccinated dogs (n = 30), non-vaccinated dogs (n = 15), vaccinated cats (n = 30), and non-vaccinated cats (n = 15). Animals in the vaccinated groups were vaccinated intramuscularly on days 0 (first dose), 21 (second dose), and 49 (booster dose). CBC, blood chemistry, and SARS-CoV-2 antibody ELISA tests were performed seven days before the first vaccination and 14 days after the final vaccination to evaluate clinical signs and immunogenicity. To assess long-term antibody persistence, ELISA were conducted on 20 vaccinated animals at 4, 8, and 12 weeks post-final vaccination. The figure was created with BioRender.com, accessed on 2 February 2025.
RT-qPCR
Viral loads of SARS-CoV-2 in lung tissues and swab samples were quantified by RT-qPCR. Briefly, 1 gram of lung tissues from each dog was placed into soft tissue homogenizing CK14 tubes (Precellys, Betin Technologies, Montigny-le-Bretonneux, France) prefilled with ceramic beads and 1mL DMEM, then homogenized using a Bead blaster 24 (Benchmark Scientific, Sayreville, NJ, USA). Swab samples were placed in microtubes containing 1mL DMEM supplemented with antibiotics and suspended by vortexing. Viral RNA was extracted from both homogenized tissues and swab suspensions using the QIAamp viral RNA Mini Kit (Qiagen, Redwood, CA, USA) according to the manufacturer’s protocol.
RT-qPCR was performed using the SARS-CoV-2 Real-Time Detection Kit (SD Biosensor®, South Korea) and the CFX96 Touch Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA). The assay utilized three fluorescence channels: FAM, HEX, and CY5, corresponding to target detection and internal controls (FAM for the SARS-CoV-2 RdRp gene, HEX for the SARS-CoV-2 E gene, and Cy5 for internal control). Viral RNA copy numbers were analyzed based on the Ct values of the RdRp gene.
Blood chemistry analysis
Given that SARS-CoV-2, particularly the Delta variants, is an emerging virus with limited data on its clinical manifestations in companion animals, a comprehensive blood chemistry analysis was conducted to evaluate systemic responses and potential effects on major organ systems. The analysis also assessed possible adverse effects of the developed vaccine candidates27.
Using an automated blood chemistry analyzer, values of TP, ALP, ALT, AST, LDH, CK, CREA, BUN, BUN/CREA, and GLU were measured to evaluate systemic responses following viral infection. Additionally, TP, ALB, GLU, BUN, CREA, ALT, ALP, CHOL, TG, CA, IP, and GLO were analyzed to assess potential vaccine-related adverse effects. These parameters collectively provided insights into hepatic and renal function, metabolic status, and muscle integrity28.
TP is a key indicator of nutritional status and hepatic or renal function. Abnormal TP levels may indicate hepatic cirrhosis, nephrotic syndrome, or malnutrition. ALP serves as a marker of hepatic function, bone metabolism, and bile duct health. Elevated ALP levels may suggest hepatic or bone disorders. ALT and AST are critical enzymes for detecting liver injury. ALT, predominantly expressed in the liver, increased in response to hepatic inflammation such as hepatitis or fatty liver disease. AST is also present in the heart and muscles, making it useful for detecting muscle injuries or cardiac issues in addition to hepatic disease. LDH is a marker of general tissue damage and may increase in conditions such as hemolytic anemia, hepatic disease, or muscle injury. CK primarily reflects muscle injury, including muscular dystrophy or viral myositis. CREA and BUN are essential for evaluating renal function, while the BUN/CREA ratio helps distinguish between prerenal and renal causes of renal dysfunction. GLU is analyzed to assess glucose metabolism and detect diabetes or metabolic abnormalities. ALB reflects hepatic function and nutritional status, as it is synthesized in the liver and helps maintain plasma oncotic pressure. CHOL and TG levels serve as indicators of lipid metabolism and cardiovascular risk. CA and IP are critical for bone metabolism, and their imbalance may reflect parathyroid or vitamin D disorders. GLO is a key determinant of immune status, and altered levels may suggest immune dysregulation or hepatic disease.
Complete blood count
Blood was collected from all companion animals seven days before the first vaccination and 14 days after the final vaccination to evaluate hematological responses. Samples were immediately processed to preserve cellular integrity. CBC parameters measured included WBC, RBC, HGB, HCT, MCV, MCH, MCHC, PLT, RDW, MPV, NE%, LY%, MO%, EO%, and BASO%29.
WBCs are indicators of immune response, as changes in WBC levels can indicate infection or inflammation. RBC, HGB and HCT are critical for evaluating oxygen-carrying capacity and anemia. MCV, MCH and MCHC provide diagnostic insight into red blood cell morphology and hemoglobin content. PLT and MPV reflect coagulation status. RDW indicates red blood cell size variability, which can be indicative of underlying nutritional deficiencies or chronic diseases. Differential counts (NE%, LY%, MO%, EO% and BASO%) provide additional insight into immune response. Monitoring these parameters ensured vaccine safety30.
Cells and viruses
African green monkey kidney epithelial cells (VERO C1008, ATCC, CRL-1586) were obtained from the American Type Culture Collection (ATCC). Cells were maintained at 37 °C in air enriched with 5% CO2 using DMEM supplemented with 5% FBS, 1% penicillin (100 units/mL)-streptomycin (100 µg/mL), and 2mM L-glutamine. SARS-CoV-2 Wuhan strain and Delta variant (NCCP 43390, B.1.617.2 lineage) were provided by the National Culture Collection for Pathogens (NCCP) in Korea, and propagated in Vero cells.
SN test
For the SN test, sera were collected and stored at − 80 °C until use. Cells were seeded in 96-well plates at a concentration of 1 × 106/mL. Test sera were heat-inactivated at 56 °C for 30 min and serially diluted twofold in flat-bottom 96-well plates using PBS. Equal volume of virus suspension was added with a 1:1 ratio after dilution to 100 TCID50/well and incubated for one hour at 37 °C. The serum-virus mixtures were then added to the prepared cell monolayers and incubated at 37 °C with 5% CO2 for 3–5 days. Neutralization activity was assessed by observing the cytopathic effects (CPE). The experiment was performed in duplicate.
Histopathology
In the infection experiment with laboratory animals, all beagle dogs were euthanized and sacrificed by intravenous administration of 0.1 mg/kg pancuronium bromide and 0.1 M KCl at DPI7. Lungs and lymph nodes were examined for gross lesions, then fixed in 10% neutral-buffered formalin for one week and embedded in paraffin. Sections (4µm) were mounted on slides, deparaffinized in xylene, rehydrated through graded ethanol, and stained with hematoxylin and eosin. For IHC, sections were treated with 3% H2O2 in PBS for 20 min to block endogenous peroxidase, then subjected to antigen retrieval in 10 mM citrate buffer (pH 6.0) for one hour. Slides were incubated overnight at 4℃ with the SARS Nucleocapsid Protein Antibody (NB100-56576, Novus, USA) at a 1:200 dilution. After washing, slides were incubated with the secondary antibody (EnVision™ Detection Systems Peroxidase/DAB, Rabbit/Mouse, Dako, Denmark) for 40 min at 37℃. Color development was achieved using 3,3’-diamino-benzidine tetrahydrochloride (DAB; K5007, Dako, Denmark), followed by hematoxylin counterstaining. Sections were examined under a BX53 microscope (Olympus, Japan).
SARS-CoV-2 antibody detection by ELISA
Neutralizing antibodies against SARS-CoV-2 were quantified using the HBelisa SARS-CoV-2 Neutralizing Antibody Detection Kit (HBhealthcare, South Korea), based on a surrogate virus neutralization test (sVNT) with a competitive ELISA format. Serum samples were collected and stored at -20 °C until analysis, then diluted according to the manufacturer’s protocol. Plates pre-coated with SARS-CoV-2 RBD were incubated with diluted samples for 30 min at room temperature to allow antibodies to bind to the antigen. ACE2-biotin conjugates, streptavidin-horseradish peroxidase (HRP), and tetramethylbenzidine (TMB) substrate were added each with incubation and washing steps. The reaction was stopped by adding stop solution and the absorbance was read at 450 nm using a microplate reader. In this assay, neutralizing antibodies in serum compete with ACE2-HRP binding to the coated antigen. Thus, higher antibody concentrations result in lower O.D. values. Results were interpreted by the ratio of the O.D. value of the sample to the calibrator. If the ratio is 0.8 or higher, it is judged as negative (neutralizing antibodies to SARS-CoV-2 are not detected), and if it is less than 0.8, it is judged as positive (neutralizing antibodies to SARS-CoV-2 are detected).



















Leave a Reply