Key Takeaways
- Early-stage melanoma generally has a good prognosis and is often curable.
- Surgery is the most common treatment for stage 0 through stage 2 melanoma.
- Radiation and immunotherapy may be options if surgery isn’t available or in specific cases.
Early-stage melanoma (0, 1, or 2) generally means your prognosis is good. Stages are how healthcare providers determine how far cancer has progressed, whether it has spread, and what that may mean for outcomes.
Melanoma is an aggressive form of skin cancer, but it is often curable in the early stages. From immunotherapy drugs to surgery, there are several possible treatment options that can be used, depending on the stage.
DermNet / CC BY-NC-ND
Stage 0 (In Situ) Melanoma
Stage 0 is the earliest stage of melanoma. In this stage, symptoms may be subtle, such as the appearance of a flat or slightly raised spot on your skin or a mole that changes appearance. Early stage melanoma doesn’t usually cause the same symptoms that might be present in later stages, like weight loss or feeling unusually tired.
Stage 0 melanoma, often called “in situ” lesions, means cancer cells are localized and haven’t spread. Unlike invasive melanoma, rates of in situ melanoma are increasing in the United States.
Treatment typically involves surgery to remove the cells, along with about a half-centimeter (cm) of surrounding normal skin, called the margin, to ensure all cancer cells are excised.
Radiation therapy may be used if surgery isn’t possible.
The drug imiquimod, an immunotherapy cream, might be used off-label to boost the body’s immune response against cancer cells. It’s suitable for early-stage treatment and may be effective for areas like the face where surgery could affect appearance.
Some studies suggest that imiquimod may be effective in treating melanoma in situ in parts of the body where surgery may need to be avoided for cosmetic reasons, such as the face.
Stage 1 Melanoma
Stage 1 melanoma is broken down into two categories, which are based on a value called the Breslow thickness. This measures the depth of the melanoma in the layers of the skin, with lower numbers suggesting less chance the melanoma will spread.
Stage 1A includes lesions 0.8 millimeters (mm) thick or less.
Stage 1B refers to tumors either less than 0.8 mm thick with ulceration or 0.8 to 1.0 mm thick with or without skin damage from ulceration.
Treatment typically involves surgically removing the melanoma and 1 cm to 2 cm of surrounding skin. In most cases, this procedure can be done at an outpatient clinic or healthcare provider’s office.
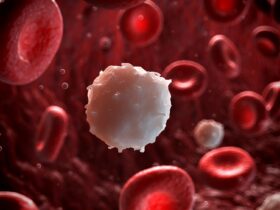
If a stage 1 melanoma is more than 1 mm thick, a lymph node dissection or biopsy might be performed, as cancer can spread via lymph nodes. This procedure aids in precise staging and treatment planning.
Breslow Thickness
The Breslow thickness helps to determine 5-year survival rates for melanoma. These survival rates are averages and may not reflect your individual case. If the melanoma size is:
- Less than 1 mm: Around 95% of people will be alive five years after being diagnosed
- 1 to 2 mm: The five-year survival rate is around 90%
- 2 to 4 mm: The five-year survival rate drops to about 77%
- Greater than 4 mm: The five-year survival rate is around 65%
Stage 2 Melanoma
Stage 2 melanoma involves larger cancer growths than stage 1, but the cancer hasn’t spread to other parts of the body. Substages for stage 2 include lesions up to 4 mm thick.
Surgical removal is the standard treatment, and the amount of normal skin removed depends on the melanoma’s size. If the melanoma is:
- Between 1 mm and 2 mm thick, 1 cm to 2 cm of healthy skin will be excised
- Between 2 mm and 4 mm thick, 2 cm of healthy skin will be excised
A sentinel node biopsy also allows the surgeon to determine if a melanoma has begun to spread, which may change the assigned cancer stage. It is often recommended for stage 2 melanoma, and occasionally for stage 1 as well.
In this procedure, a weak radioactive dye is injected into the melanoma. It is used to trace through the lymphatic system and identify the sentinel nodes, which are closest to the cancer and most likely to be affected first if the cancer spreads.
In stage 2 melanoma, your healthcare provider may also consider immunotherapy drugs as a treatment option after surgery. However, the evidence is limited on how effective these drugs or radiation treatments may be in this case.
Immunotherapy drugs that may benefit people with some stage 2 cancers include:
- Keytruda (pembrolizumab)
- Opdivo (nivolumab)
- Tecentriq (atezolizumab), in cases involving a specific BRAF V600 gene mutation and when used in combination with Cotellic (cobimetinib) and the chemotherapy drug Zelboraf (vemurafenib)
















Leave a Reply